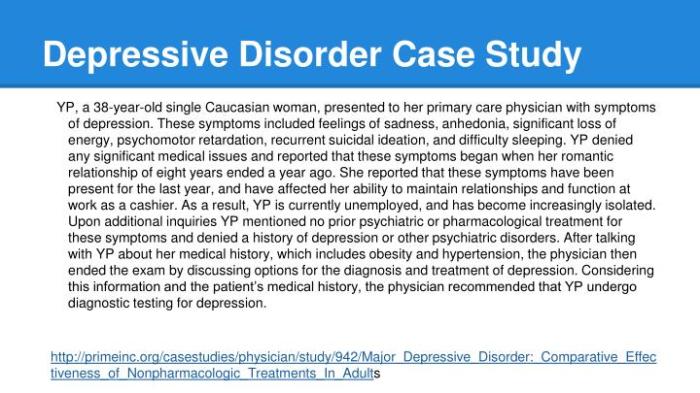
Major depressive disorder hesi case study – Major depressive disorder (MDD) is a prevalent mental health condition characterized by persistent sadness, loss of interest, and a range of debilitating symptoms. This HESI case study delves into the intricate presentation, assessment, diagnosis, and treatment of MDD, providing a comprehensive understanding of this complex disorder.
The case study explores the interplay of biological, psychological, and social factors that contribute to MDD, shedding light on its etiology. It also examines the efficacy of various treatment modalities, including pharmacological interventions, psychotherapy, and alternative therapies, highlighting the challenges and successes encountered in the treatment process.
1. Definition of Major Depressive Disorder (MDD): Major Depressive Disorder Hesi Case Study
Major Depressive Disorder (MDD) is a prevalent mental health condition characterized by a persistent state of low mood, loss of interest, and a range of cognitive, behavioral, and physical symptoms. It is a serious and debilitating condition that can significantly impair an individual’s daily functioning, relationships, and overall well-being.
Key Symptoms and Diagnostic Criteria
- Persistent low mood (depressed mood) most of the day, nearly every day.
- Loss of interest or pleasure in activities that were once enjoyable.
- Significant changes in appetite (weight gain or loss).
- Sleep disturbances (insomnia or hypersomnia).
- Psychomotor agitation or retardation.
- Fatigue or loss of energy.
- Feelings of worthlessness or excessive guilt.
- Difficulty concentrating or making decisions.
- Recurrent thoughts of death or suicide.
Prevalence and Impact
MDD is a common mental health disorder, affecting approximately 17% of the population at some point in their lives. It is more prevalent in women than men and often occurs in conjunction with other mental health conditions, such as anxiety disorders.
The impact of MDD on individuals and society is significant. It can lead to impaired work performance, strained relationships, and decreased quality of life. MDD is also associated with increased healthcare utilization, disability, and mortality.
2. Assessment and Diagnosis of MDD
Assessment Tools and Methods
The assessment and diagnosis of MDD typically involve a comprehensive evaluation that includes:
- Clinical Interviews:A detailed conversation between a mental health professional and the individual, exploring their symptoms, history, and current functioning.
- Self-Report Measures:Standardized questionnaires or rating scales, such as the Beck Depression Inventory (BDI) or the Patient Health Questionnaire (PHQ-9), which assess the severity and duration of depressive symptoms.
- Physical Examinations:To rule out any underlying medical conditions that may be contributing to the symptoms.
Differential Diagnosis, Major depressive disorder hesi case study
MDD must be differentiated from other mental health conditions that may share similar symptoms, such as:
- Bipolar Disorder:Characterized by alternating episodes of depression and mania or hypomania.
- Anxiety Disorders:May present with symptoms of anxiety, worry, and fear, but typically lack the persistent low mood and loss of interest seen in MDD.
- Personality Disorders:May have persistent patterns of negative thinking or behavior, but do not typically meet the full diagnostic criteria for MDD.
3. Etiology of MDD
Biological Factors
- Neurotransmitters:Dysregulation of neurotransmitters, such as serotonin, norepinephrine, and dopamine, is thought to play a role in MDD.
- Genetic Factors:MDD has a strong genetic component, with studies suggesting a heritability rate of around 37%.
Psychological Factors
- Personality Traits:Certain personality traits, such as neuroticism and pessimism, have been linked to an increased risk of developing MDD.
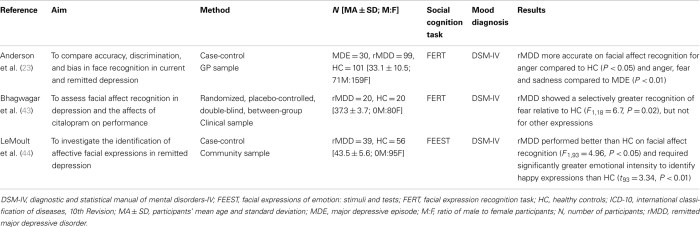
- Cognitive Biases:Individuals with MDD often exhibit cognitive biases, such as negative self-perceptions, catastrophizing, and rumination.
Social Factors
- Environmental Stressors:Traumatic events, chronic stress, and lack of social support can contribute to the development of MDD.
- Social Determinants of Health:Factors such as poverty, unemployment, and discrimination can increase the risk of MDD.
Theories and Models
Various theories and models attempt to explain the development of MDD, including:
- Monoamine Hypothesis:Proposes that MDD is caused by a deficiency of monoamine neurotransmitters, such as serotonin and norepinephrine.
- Cognitive-Behavioral Model:Emphasizes the role of negative thoughts, beliefs, and behaviors in the development and maintenance of MDD.
- Psychodynamic Model:Focuses on unconscious conflicts and early life experiences that may contribute to the development of MDD.
4. Treatment of MDD
Pharmacological Interventions
Antidepressants are commonly used to treat MDD. These medications work by increasing the levels of neurotransmitters in the brain, such as serotonin or norepinephrine.
- Selective Serotonin Reuptake Inhibitors (SSRIs):Commonly prescribed first-line antidepressants, such as fluoxetine (Prozac) and sertraline (Zoloft).
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs):May be effective in treating MDD with associated anxiety symptoms, such as venlafaxine (Effexor) and duloxetine (Cymbalta).
- Tricyclic Antidepressants (TCAs):Older antidepressants that are still used in some cases, such as amitriptyline (Elavil) and imipramine (Tofranil).
- Mood Stabilizers:May be used to treat MDD in individuals with bipolar disorder or who do not respond well to antidepressants, such as lithium and valproate.
Psychotherapy
Psychotherapy is an important component of MDD treatment. It can help individuals understand and manage their symptoms, develop coping mechanisms, and improve their overall well-being.
- Cognitive-Behavioral Therapy (CBT):Focuses on identifying and changing negative thoughts and behaviors that contribute to MDD.
- Interpersonal Therapy (IPT):Addresses interpersonal problems and relationships that may be contributing to MDD.
- Psychodynamic Therapy:Explores unconscious conflicts and early life experiences that may be influencing the development and maintenance of MDD.
Alternative and Complementary Treatments
In addition to pharmacological interventions and psychotherapy, there are a number of alternative and complementary treatments that may be beneficial in the treatment of MDD, such as:
- Exercise:Regular physical activity has been shown to improve mood and reduce depressive symptoms.
- Mindfulness:Mindfulness-based interventions, such as meditation and yoga, can help individuals manage stress and improve their overall well-being.
- Light Therapy:Exposure to bright light can be effective in treating seasonal affective disorder (SAD), a type of MDD that occurs during the winter months.
Expert Answers
What are the key symptoms of MDD?
Persistent sadness, loss of interest, changes in appetite or sleep, fatigue, difficulty concentrating, feelings of worthlessness or guilt.
How is MDD diagnosed?
Through a clinical interview, self-report measures, and physical examination, meeting specific diagnostic criteria Artikeld in the DSM-5.
What are the common treatment options for MDD?
Pharmacological interventions (antidepressants, mood stabilizers), psychotherapy (CBT, IPT, psychodynamic therapy), and alternative therapies (exercise, mindfulness, light therapy).
